Postgraduate education in the world and Ukraine
- 3.1. Historical trends
- 3.2. Conditions for harmonization of CPD
- 3.3. Basic principles of CPD
- 3.4. Experience of accreditation of CPD systems
Training of physicians in the world
WHO experts note that today in Europe there is no generally accepted approach to continuing medical education, but there is a general agreement that the quality of medical services directly depends on the constant maintenance of physicians` competencies during the procedures of continuous improvement and assessment of their qualifications. It is also emphasized that it is of great importance to ensure (and improve) the quality and academic requirements of the providers of educational services or training programs, on the basis of which physicians coordinate their own educational plans.
The most important prerequisite for ensuring the mandatory nature of continuing professional development is the creation of a unified accreditation system for service providers and programs, as well as the "collective responsibility" of all participants in the medical training system.
The general scheme of medical training in Europe is as follows:
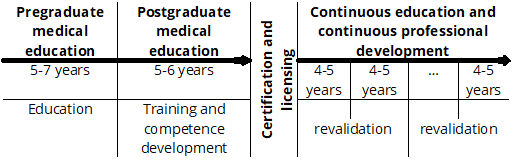
According to the World Federation for Medical Education (WFME), postgraduate medical education is the phase of medical training when physicians gain experience after obtaining a basic medical qualification. This phase of training is conducted in accordance with specific rules and regulations.
Postgraduate medical education includes preparation for official registration, industrial/professional training, specialization and subspecialization, as well as other formalized training programs appropriate to the performance of certain expert functions.
Postgraduate education is a part of the learning continuum in medicine, also included in continuing medical education (CME) or continuing professional development (CPD).
There are a number of CPD models in the world:
One-stage: after obtaining a medical degree - an internship or residency (e.g., Germany, Israel, Romania, Moldova, etc.)
Two-stage: after obtaining a medical degree - an internship and then a residency or specialization (e.g., Ukraine, Sweden, UK, Poland, etc.)
Three-stage: after obtaining a medical degree - an internship or internship training, followed by residency, and then specialization in a narrow specialty (e.g., the United States, France, etc.)
According to the World Federation of Medical Education (WFME), continuous professional development (CPD) refers to the period of education and training of physicians that begins after completion of basic medical education and postgraduate training and continues thereafter throughout the professional life of each physician.
CPD is considered a professional obligation of every physician and is a prerequisite for improving the quality of medical care. CPD is fundamentally different from the two previous formal phases of medical education - basic medical education and systematic postgraduate medical training. While the last two are conducted in accordance with specific rules and regulations, CPD is mainly based on self-study and experiential learning rather than on training under someone's guidance.
CPD is aimed at maintaining and improving the expertise (knowledge, skills and attitudes) of the individual physician, which is vital for meeting the changing needs of patients and the healthcare delivery system, in line with new findings in medical research.
In order to stimulate the participation of all physicians in continuing education and increase their level of responsibility, Europe is considering the introduction of the principle of mandatory participation in systems or programs of continuous medical education (CME). It is emphasized that it is of great importance to ensure (and improve) the quality and requirements for the academic level of educational service providers or training programs, on the basis of which physicians draw up and implement their own educational plans that meet the specifics of their practice and take into account their needs.
The medical training systems in Europe and America are currently making attempts to harmonize on the following principles:
- educational credits are accumulated continuously with annual control;
- continuing medical education (CME) is an obligation through the mechanisms of licensing and certification of medical professionals, as well as the remuneration system. The condition for obtaining and renewing a specialist certificate is the annual completion of a set number of credits;
- amid the active participation of professional societies, state regulation of the CME is reinforced through quality control of medical care (safety and effectiveness of patient treatment);
- publicity of information about the quality of physicians' work is ensured, for example, through open registers of physicians with information about their educational activity, ratings of physicians and medical institutions, etc.
In many countries, the CME system is mandatory, with periodic revalidation procedures that confirm a physician's right to continue practicing medicine.
The differences between CME models are partly driven by a wide variety in aspects such as the structure of health care systems, medical education models, accreditation systems, socioeconomic concepts, and geographic conditions. But despite these differences, there are a number of common features:
- many models use credit systems (e.g., hours of educational activities are equated to credits);
- educational activities are divided into the following categories: "live" activities, or off-the-job training (e.g., courses, seminars); on-the-job training (e.g., activities based on own practice, clinical reviews); studying reusable materials (e.g., printed materials, CDs);
- in systems where recertification is mandatory, demonstration of ongoing learning maintenance is a requirement.
However, the high importance of informal methods of CPD does not in any way diminish the role of systematic formal methods of training: refresher courses, conferences, etc. Moreover, medical professional organizations and licensing authorities propose (and often enshrine in legislation) mechanisms for quality control of training, determine the number of certified CPD courses, the required amount of training for physicians, and the assessment of physicians upon completion of the CPD course. It is considered that the best way to meet the needs of physicians, given the differences in their professional responsibilities, goals and objectives of training, is a multifaceted system of CPD, which provides for different methods of training.
Thus, mandatory participation in continuing education is considered to be a value recognized by physicians and society, but this does not mean that the systems that are being developed in Europe will necessarily look the same for all physicians. Ideally, CPD systems should:
- promote the development of skills and competencies that allow for lifelong learning;
- correspond to the practice profile of the physician in training;
- meet the needs (conscious and unconscious) of the professional activity of everyone involved in continuing education (for example, help to eliminate gaps in knowledge, skills or performance of professional functions)
- provide for continuous evaluation of how an individual physician or healthcare team performs their professional activities (e.g., audit with feedback).
Therefore, participation in mandatory CME systems is promoted as a response to public expectations, professional necessity and regulatory requirement.
In the United States, the Accreditation Council for Continuing Medical Education (ACCME®), a non-profit corporation responsible for accrediting institutions that offer continuing medical education (CME) for physicians and other healthcare professionals, plays a key role in regulating the CPD system. ACCME accredits US and international institutions.
3.1. Historical trends
Historical trends in improving the system of training and certification of medical personnel in the world
Modern medicine is being improved at an extremely fast pace, and accordingly, the skills and knowledge of physicians are rapidly becoming outdated.
An analysis of the relationship between professional experience and the quality of medical care conducted in Europe in the mid-19th century showed that in 52% of cases, physicians with long work experience provide lower quality medical care. An expert review of 62 studies showed that the risk of providing low-quality care to patients increases with the length of a physician's practice. This suggests that older healthcare professionals and practicing physicians do not have a large amount of up-to-date knowledge and their knowledge becomes outdated over the years.
Based on the data obtained, in a number of countries, society has begun to put forward higher requirements for practicing physicians to be able to confirm their compliance with accepted professional standards. To this end, in many countries, physicians are required to participate in continuing education programs based on two key aspects: (a) maintaining the required level of professional competence through continuing medical education and professional development and (b) further verification of acquired skills and knowledge through various assessment and feedback mechanisms (recertification or revalidation).
In 2000, 24 commissions of the non-profit public professional organization American Board of Medical Specialties (ABMS) decided to conduct regular recertification of physicians (the so-called recertification of physicians) by approving the Maintenance of Certification® Program]. This decision was justified by the need to bridge the gap between the requirements of society to improve the quality of medical care and the low level of professional competence of physicians.
The Maintenance of Certification® Program was finally implemented in 2006. Currently, about 85% of all US physicians are certified by one of the twenty branches of the American Board of Medical Specialties, covering 145 medical specialties.
Recertification of physicians in the United States is carried out once every 8 years, in the United Kingdom - once every 5 years. In order to successfully pass recertification, a physician must provide an official certificate that he or she has annually attended 50 lecture hours of continuing medical education (CME) on the specified topic of the certification cycle, and 25 of these hours must be in the specialty. Thus, a certified American physician submits to the commission an official written confirmation of having a total of 400 hours of continuing medical education at the end of the eight-year certification cycle.
In addition, every year, the physician is required to undergo a self-assessment and provide satisfactory answers to 50 questions on a questionnaire approved by the Board of Certification in the specialty. Information on the results of the annual examination self-assessment is reported to the American Board of Physicians of various specialties during 8 years.
In the last year of the eight-year cycle, the physician must apply for recertification and successfully answer 100 questions of the test, using a written or computerized form of answer options developed by the American Board of Physicians of various specialties (ABPS).
The World Federation of Medical Education also noted the importance of repeated (periodic) certification of physicians as a guarantee of quality assurance of CPD for physicians in 2003.
In many Western European countries, the issues of continuing education are regulated by professional medical organizations.
For example, in France, three professional bodies are involved in the process, the so-called National Councils for Continuing Medical Education (Conseils Nationaux de Formation Médicale Continue) - the Council for Ambulatory Care Physicians, the Council for Freelance Ambulatory Care Physicians, and the Council for Attending Physicians.
In the Netherlands, since 2005, recertification has been a condition for maintaining membership in the medical register: physicians are obliged to systematically participate in continuing medical education programs and undergo peer review every five years.
In Germany, physicians are licensed to practice by regional ministries and regulated by regional chambers (professional associations). The recertification scheme adopted in Germany requires physicians to accumulate a set amount of participation in continuing medical education programs (250 credits, where 1 point is approximately 45 minutes of training) every five years.
In Austria, the Diplom-Fortbildungs-Programm (continuing medical education program) for licensed physicians was approved in December 2001. Physicians must accumulate 150 continuing medical education credits, 120 of which must be obtained in certified programs related to the physician's specialty and at least 40 credits in the physician's own specialty. The Austrian Medical Chamber is responsible for compliance with these requirements. The training units of the Austrian Academy of Physicians are responsible for the practical implementation of the program. According to the Chamber, the system of continuing medical education should be independent, internationally competitive, meet high scientific standards and be free from economic interest.
In Belgium, general practitioners and specialists are required to submit a certificate of 20 hours of continuing medical education within a year in programs recognized by the general practitioner licensing committee. The National Institute for Sickness and Disability Insurance grants accreditation if the physician's activities meet additional requirements, including participation in continuing medical education programs and peer reviews. Accreditation is valid for three years. To renew it, specialists and general practitioners must submit 200 credits of participation in continuing medical education programs and pass at least two peer reviews during the year.
In France, a system of continuing medical education and medical audits (assessment of professional practice) with participation assessment every five years were introduced in 2004 as mandatory.
Thus, the CME systems of many countries have evolutionarily reached such stages of their development when they began to require professionals not only to constantly improve in a controlled manner, but also to constantly confirm their professionalism.
3.2. Conditions for harmonization of CPD systems
In the EU countries, attention is drawn to the problems associated with the rapid increase in the volume of medical information and the frequency of adverse events that affect the quality of care and patient safety. There is also a dissonance between the expectations of patients and the capabilities of the physicians who treat them, resulting in problems in problems in relations between the public and professional community. This gives groundstode demand that physicians increase their responsibility for improving their competence through continuing education programs.
For example, the World Federation for Medical Education (WFME) emphasizes that participation in CPD is a professional duty of a physician and a condition for improving the quality of medical care. The Standards developed by the WFME statethatinordertoprovide the highest quality medical care, the CPD systemshouldbeaimedatincreasingtheimportanceandexperience (both clinical and theoretical) of the physician, teaching organizational skills (creating and leading a group of specialists), developing communication, teaching, research and administrative skills, and mastering the provisions of medical ethics. In addition, the system of professional training has to prepare physicians to solve clinical problems that are not yet known at the time of training, so it should not only fill the identified gaps in the clinical education of physicians, but also provide them with a wide range of knowledge and experience.
An obstacle to joint efforts aimed at achieving harmonization of CME in all EU Member States is the diversity of CME systems. At present, there is no consistent approach or agreement on how continuing education in the course of medical practice should be organized, structured, implemented, documented and regulated.
The same lack of uniformity is observed in the governance of CME systems: it is organized either at the local or national level, although national-level governance is more common. The general principle remains that the primary responsibility for CPD lies with the medical community. The complexity of the CME system in the EU is compounded by differences in the roles of public authorities and medical associations in individual Member States, as well as language difficulties.
In some countries, CPD is conducted in specialized institutes; some of them are private and operate on a commercial basis, which is evidence of the growing market for medical education. Other institutions are governmental, and often provide systematic specialized (postgraduate) training in addition to CPD courses. Another option for the provision and development of CPD is provided by national medical councils or academies. In some countries (e.g. France), CPD for a large number of physicians is provided on the basis of legislation regulating the labor market.
The diversity of CME systems in Europe creates challenges for both healthcare professionals and governments, especially with regard to physician movements from one country to another and practice requirements.
This diversity, especially in the EU, is increasingly becoming an obstacle for those who are investing time and money in achieving harmonization of CME across all member states. In order to create equivalent national CME systems, experts suggest addressing several issues related to educational infrastructure, without which it is considered impossible to successfully implement the desired strategic approaches.
The most important is the mutual agreement and recognition by all physicians, stakeholders and medical societies in any European country that participation in formal CME and, more broadly, the pursuit of continuing education is a necessary professional and ethical obligation.
In order for physicians to improve their qualifications in different countries with full confidence, there must be an identity of accreditation standards between countries. There should be the same principles and results of accreditation of service providers and organizers of CME/CPD. With such uniformity, physicians who wish to undergo training that is not provided in their own country will be able to undergo it in another country and it will be considered equivalent in content, outcomes and quality to similar programs organized in their country.
The differences between CME models are partly driven by a wide variety in aspects such as the structure of health care systems, medical education models, accreditation systems, socioeconomic concepts, and geographic conditions. But despite these differences, there are a number of common features:
- many models use credit systems (e.g., hours of educational activities are equated to credits);
- educational activities are divided into the following categories: "live" activities, or off-the-job training (e.g., courses, seminars); on-the-job training (e.g., activities based on own practice, clinical reviews); studying reusable materials (e.g., printed materials, CDs);
- in systems where recertification is mandatory, demonstration of ongoing learning maintenance is a requirement.
However, the high importance of informal methods of CPD does not in any way diminish the role of systematic formal methods of training: refresher courses, conferences, etc. Moreover, medical professional organizations and licensing authorities propose (and often enshrine in legislation) mechanisms for quality control of training, determine the number of certified CPD courses, the required amount of training for physicians, and the assessment of physicians upon completion of the CPD course. It is considered that the best way to meet the needs of physicians, given the differences in their professional responsibilities, goals and objectives of training, is a multifaceted system of CPD, which provides for different methods of training.
Thus, mandatory participation in continuing education is considered to be a value recognized by physicians and society, but this does not mean that the systems that are being developed in Europe will necessarily look the same for all physicians. Ideally, CPD systems should:
- promote the development of skills and competencies that allow for lifelong learning;
- correspond to the practice profile of the physician in training;
- meet the needs (conscious and unconscious) of the professional activity of everyone involved in continuing education (for example, help to eliminate gaps in knowledge, skills or performance of professional functions)
- provide for continuous evaluation of how an individual physician or healthcare team performs their professional activities (e.g., audit with feedback).
Therefore, participation in mandatory CME systems is promoted as a response to public expectations, professional necessity and regulatory requirements.
A group of leaders of accreditation systems for CME in several EU Member States, the United States of America and Canada (the Rome Group) has begun to prepare an agreed statement that highlights consensus on the core (fundamental) values and responsibilities underlying substantive equivalence of CME systems. This statement indicates that the accreditation systems of the CME/CPD should :
1) contribute to the improvement of the quality of physicians' professional functions and thereby to the promotion of public health and
2) be based on information related to the educational needs of physicians and ultimately be aimed at helping physicians to strengthen the health of the population.
"The Rome Group", in developing the concept of promoting globalization, reciprocity and equivalence of accreditation and credentialing systems in the field of CME and CPD, developed an agreement on the need to bring existing national CME and CPD accreditation systems, service providers and organizers of these activities, as well as credentialing systems to reasonable uniformity in terms of the principles and results of accreditation. This concept is based on the following structural components:
1) physicians participating in educational projects (CPD);
2) service providers and organizers of educational activities (or events)
3) accreditation organizations that certify that service providers and organizers of educational activities meet certain accreditation standards and therefore can be awarded credit points for participation in these activities.
Representatives of organizations that are part of the accreditation system of the CME/CPD and credit awarding of Bulgaria, Canada, France, Germany, Italy, Spain, Spain, the United Kingdom, the United States of America and the EU came to a consensus that the implementation of CME/CPD systems based on this concept will lead to mutual recognition and the establishment of the principle of reciprocity while preserving the cultural and historical uniqueness of each system.
3.3. Main principles of CPD
The main principles underlying the system of organization of CPD in some European countries are as follows:
- The responsibility for monitoring and decision-making and the development of the CPD system is vested in the CPD Committee of the Federation of Royal Colleges of Physicians.
- Individual CPD activity is planned by the physician in advance through a personal development plan and should reflect and correspond to the current and future profile of the physician's professional practice and performance.
- Each cycle of formal training is accompanied by a formalized document "Declaration on Prevention of Conflict of Interest". Any competition or conflict of interest on the part of participants and organizers should be declared in the training program.
- Effective CPD schemes are flexible and largely based on self-assessment.
- The standards for CPD documentation required for recertification are set by colleges or faculties.
- Some educational activities may not be endorsed by a formal certification system, but in this case it is the responsibility of the individual to document their activities and knowledge.
- Self-accreditation of relevant activities and documentation of learning that reflects local and national practice needs and the individual's own training needs should be allowed and encouraged.
- The registration of CPD credits obtained by a physician is carried out online, through which he or she has access to an individual diary (portfolio).
- Providers of approved "external" educational services are encouraged to keep records of participants for five years in order to facilitate the process of random audits that may be conducted by faculties and colleges
- Every year, selectively, Colleges/Faculties should carry out selective control of the activities of participants in the educational process, including through the verification of 5% of entries in the diaries (structured portfolio) of all participants of the CPD.
- The categories of credits are defined: a) clinical; b) non-clinical - educational activities that are not directly related to clinical issues, such as management courses, ethical and legal issues, evaluation of training; c) external - for activities outside the hospital; d) internal - includes activities within the hospital or organized by the hospital or provided exclusively for local physicians.
- A physician must accumulate 50 credits per year (1 credit corresponds to 1 hour of educational activity), which is confirmed by annual and then 5-year certificates.
- Of the 250 CPD credits that a physician must accumulate in five years, at least 125 must be external clinical credits and at least 25 must be external non-clinical credits.
- All CPD activities must be officially approved/recognized for quality and meet the following criteria:
- organizers must indicate any commercial interests of speakers and presenters;
- any commercial sponsorship or interests of the program planning organization, representatives, or coordinators must be declared in the registration form and this support must not influence the structure or content of the educational program;
- organizers must include information about the objectives of the event and how it will be applied in practice;
- organizers must provide a detailed program of the event, which should include an hourly schedule and a brief description of the session;
- The Royal College of Physicians must approve external CPD events, and only those external events that have been approved will appear online.
- Distance learning modules and programs must be reviewed and approved by the official CPD system. Successful completion of a distance learning module or program has to be confirmed by a certificate indicating the user's name and data, assessment results, and the number of credits for distance learning in the CPD.
- Education providers should "provide delegates with questionnaires to track the relevance, quality and effectiveness of the event". This evaluation should be made available to the provider and, where possible, to the supervisory authority (e.g. through the use of an online evaluation application).
- The CPD programs are approved by: a) the CPD directors of the three colleges of the Federation; b) nineteen regional CPD advisors; c) three non-clinical advisors; d) thirteen representatives of the specialties involved in the CPD programs.
- If the requirements for participation in the CPD programs are not met, or if a person does not have sufficient evidence of having received the stated minimum of CPD credits, then these individuals will be re-evaluated the following year.
- The anonymized and organized results of the screening are presented annually to the CPD Policy Committee and are regularly published in the CPD newsletter.
Denial to provide sufficient evidence to support the claimed credits will result in the credits not being approved in the annual report during the audit. In case of suspicion of falsification of evidence regarding the above activities of the CPD, a repeated inspection is carried out with the participation of the General Medical Council.
3.4. Experience of accreditation of the CPD system
To ensure the quality of the CME system, the Accreditation Council for Continuing Medical Education (ACCME) has developed standards for the recognition of providers of professional activities within the framework of CME.
The ACCME's mission is to identify, develop, and promote high national standards of CME quality that improve physician performance, including patient care and the state of health care for the public. The ACCME is supported solely by contributions from accredited providers and fees from registered workshops.
ACCME standards are designed to ensure independence in CME activities. The policies associated with the standards are aimed at facilitating the appropriate free flow of new information and scientific exchange. At the same time, the accredited independence of CME and freedom from commercial influence are maintained. The standards are recognized as a national model by public authorities and government agencies, other accredited healthcare bodies, and the professional medical community.
ACCME accreditation is a voluntary, self-regulatory system that assures the public and the medical community that accredited CME providers are strategic partners in healthcare quality and safety initiatives, providing physicians with appropriate and effective education that meets their professional education and practice needs. The accreditation standards ensure that CME is designed to be independent, free of commercial bias, and based on current best practices.
The accreditation and reaccreditation decision-making process evaluates a provider's compliance with the CME accreditation requirements. Based on these relevant findings, ACCME decides the accreditation status of the provider using various options.
ACCME has accredited approximately 700 organizations. In addition, the ACCME is recognized by 41 state and territorial medical societies and accredits approximately 1,200 state organizations offering CME. Accredited providers represent a wide range of organizations, from national specialty societies to small community hospitals. In total, nearly 1,900 accredited CME providers offer more than 148,000 activities each year.
Accredited educational events attract about 26 million healthcare professionals annually. Information about these events is disseminated through a variety of channels, including meetings and courses, medical journals, and the Internet.
Physicians participate in accredited CME activities to maintain their own education and improve their practice competencies. Participation in accredited CME also helps physicians meet the requirements for licensure, specialty board certification, accreditation, membership in professional societies, and other professional requirements.
3.4.1. Accreditation decisions
Decisions on the accreditation of providers (suppliers of the CME)
The accreditation and re-accreditation decision-making process is based on an assessment of a provider's compliance with the requirements of CME accreditation. Based on the findings, ACCME decides on the type of accreditation for the provider using one of the following five options:
Provisional accreditation is granted for a two-year period, which is awarded to first-time applicants who demonstrate compliance with accreditation criteria 1-3 and 7-12. Occasionally, a provider may be granted extended provisional accreditation for one to two years if compliance issues are identified that prohibit progress toward accreditation.
Accreditation - corresponds to a four-year term granted to accredited suppliers. Suppliers that demonstrate one or more non-compliances with accreditation criteria 1-13 are accredited, but are required to submit reports on the elimination of identified non-compliances.
Accreditation with distinction corresponds to a six-year accreditation period and is available only to suppliers seeking re-accreditation, not to initial applicants. To achieve accreditation with distinction, providers must demonstrate compliance with the accreditation criteria (1-13) and use one of two options. Providers who receive an accreditation decision after November 2019 must use Option B("Menu of new assessment criteria (C23-C38)") to achieve accreditation with distinction.
A probationary period is granted to accredited providers who have serious problems with compliance with ACCME requirements. Providers are required to submit progress reports during the probationary period. Providers with accreditation may change their status during the probationary period if their progress reports do not demonstrate that noncompliance has been corrected. Most suppliers on probation quickly make improvements, return to accreditation status, and maintain compliance. Suppliers cannot remain in this period for more than two years.
Nonaccreditation: Although decisions to not accredit are rare, ACCME will make such a decision in the following circumstances:
- The initial applicant does not meet any of the criteria necessary to achieve Provisional Accreditation.
- A provisionally accredited provider has serious problems and noncompliance.
- A supplier in a probationary period of two years cannot demonstrate in one or more reports that it has corrected deficiencies and achieved compliance with all accreditation criteria.
In rare cases, when there are compelling reasons, an accredited provider may change its non-accreditation status.
3.4.2. Accreditation criteria
Initial applicants seeking pre-accreditation must meet criteria 1, 2, 3, and 7-12 within a two-year period. Providers seeking full accreditation or re-accreditation for a four-year period must meet criteria 1-13. Providers also have the opportunity to try to achieve Accreditation with Distinction (six-year term). Providers seeking the distinction must meet criteria 1-13 and must use Option B("Menu of new assessment criteria (C23-C38)") to achieve Accreditation with Distinction.
CRITERION 1 The provider has a CME mission statement that includes the expected outcomes, articulated in terms of changes in competence, performance, or patient outcomes that will result from the program.
CRITERION 2 The provider addresses in CME activities the educational needs (knowledge, competence, or performance) that underlie the gaps in the professional practice of their trainees.
CRITERION 3 The provider develops activities/educational interventions designed to change competencies, performance, or patient outcomes as described in its mission statement.
CRITERION 4 This criterion was removed effective February 2014.
CRITERION 5 The provider selects educational formats for activities/interventions that are appropriate for the established goals and desired outcomes.
CRITERION 6 The provider develops activities/educational interventions in the context of desired physician characteristics [e.g., Institute of Medicine (IOM) competencies, Accreditation Council for Graduate Medical Education (ACGME) competencies].
CRITERION 7 The provider develops activities/educational interventions independently of commercial interests (SCS 1, 2, and 6).
CRITERION 8 The provider appropriately manages commercial facilitation (if applicable, SCS 3 of the ACCME Standards for Commercial Support of SM).
CRITERION 9 The provider ensures that commercial support is separate from education (SCS 4).
CRITERION 10 The provider actively contributes to the improvement of the healthcare system and does not promote its own commercial interests (SCS 5).
DEFINITION OF A COMMERCIAL ENTITY
A commercial entity is any person who manufactures, sells, resells, or distributes health care products or services that are consumed or used by patients. ACCME does not consider providers of clinical services directly to patients to have a commercial interest unless the provider is owned or controlled by an ACCME-designated commercial entity. A commercial entity is not subject to ACCME accreditation. Commercial entities cannot be accredited providers and cannot be joint providers. In the context of this definition, ACCME considers the following types of organizations eligible for accreditation and free to control CME content: 501-C nonprofit organizations; Government agencies, non-healthcare companies, liability insurance providers, health insurance providers, group medical practices, for-profit hospitals, for-profit rehabilitation centers, for-profit nursing homes, blood banks, diagnostic laboratories ACCME reserves the right to update this definition and list of eligible organizations from time to time without notification.
CRITERION 11 The provider analyzes the changes in learners (competence, effectiveness, or patient outcomes) achieved as a result of the overall program activities/learning activities.
CRITERION 12 The provider gathers information and conducts analysis to verify the extent to which the CME mission of the provider is being met through the delivery of CME activities/learning events.
CRITERION 13 The provider identifies, plans and implements necessary or desirable changes in the overall program (e.g., planning, faculty, infrastructure, methods, resources, facilities, interventions) that are necessary to improve the ability to fulfill the CME mission.
CRITERION 14 This CRITERION was removed effective February 2014.
CRITERION 15 This CRITERION was removed effective February 2014.
Accreditation with Distinction - Option A
CRITERION 16 The provider works to integrate CME into the process of professional practice improvement.
CRITERION 17 The provider uses non-educational strategies to further improve its performance/educational interventions (e.g., reminders, patient feedback).
CRITERION 18 The provider identifies factors outside of its control that affect patient outcomes.
CRITERION 19 The provider implements educational strategies to address, overcome, or combat barriers to improving physician competence.
CRITERION 20 The provider builds collaboration with other stakeholders through cooperation and engagement.
CRITERION 21 The provider participates in institutional or systemic quality improvement projects.
CRITERION 22 The provider is able to influence the scope and content of activities/training events.
Accreditation with Distinction - Option B
CRITERION 23 Members of interprofessional teams are involved in the planning and delivery of interprofessional continuing education (IPCE).
CRITERION 24 Patients/public representatives are involved in the planning and delivery of CME.
CRITERION 25 Healthcare trainees are involved in the planning and delivery of CME.
CRITERION 26 The provider promotes the use of health promotion information and practice data to improve the health care system.
CRITERION 27 The provider addresses factors beyond clinical care that affect population health.
CRITERION 28 The provider collaborates with other organizations to more effectively address population health issues.
CRITERION 29 The provider develops CME to optimize the communication skills of learners.
CRITERION 30 The provider develops CME to optimize the technical and procedural skills of learners.
CRITERION 31 The provider creates individualized learning plans for trainees.
CRITERION 32 The supplier utilizes strategies to support the improvement of its CME activities.
CRITERION 33 The provider participates in CME research and scholarship.
CRITERION 34 The provider supports the continuous professional development of its CME team.
CRITERION 35 The provider demonstrates creativity and innovation in the development of its CME program.
CRITERION 36 The provider demonstrates improvements in the professionalism of its attendees.
CRITERION 37 The provider demonstrates improvements in healthcare quality.
CRITERION 38 The provider demonstrates the impact of the CME program on patients or their communities.
3.4.3. ACCME standards
ACCME standards for ensuring independence in CME activities
Standard 1: Independence
STANDARD 1.1 The CME provider must ensure that the following decisions are free from the influence of commercial interests:
(a) Identification of CME needs; (b) Determination of educational objectives; (c) Selection and presentation of content; (d) Selection of all individuals and organizations that will be able to control the content of CME; (e) Selection of learning methods; and (f) Evaluation of performance.
STANDARD 1.2 A commercial entity may not assume the role of an unaccredited partner in a relationship with a joint provider.
Standard 2: Resolving conflicts of personal interest
STANDARD 2.1 The provider must be able to demonstrate that everyone who has the ability to control the content of the educational activity has disclosed all relevant financial relationships with any commercial entities to the provider. The ACCME defines a "relevant" financial relationship as a financial relationship of any amount that has occurred within the last 12 months that creates a conflict of interest.
STANDARD 2.2 An individual who refuses to disclose a relevant financial relationship will be ineligible to serve as a planning committee member, faculty member, or CME author and may not control or be responsible for the development, management, submission, and evaluation of CME activities.
STANDARD 2.3 The provider shall establish a mechanism to identify and resolve all conflicts of interest in providing educational services to students.
Standard 3: Appropriate use of commercial support
STANDARD 3.1 The provider shall make all decisions regarding the disposition and disbursement of commercial support.
STANDARD 3.2 A commercial entity cannot require a provider to accept advice or service regarding teachers, authors, participants, or other educational matters, including content, from the commercial entity as a condition of the provision of funds or services.
STANDARD 3.3 All commercial support related to the activities of the CME must be provided with the full knowledge and approval of the provider.
STANDARD 3.4 The terms, conditions, and objectives of commercial support should be documented in a written agreement with the commercial entity that includes the provider and its educational partners. The agreement shall include the provider even if the support is provided directly to the provider's educational partner or joint provider.
STANDARD 3.5 The written agreement shall identify the commercial interest that is the source of the commercial support.
STANDARD 3.6 The commercial entity and the provider shall sign the written agreement.
STANDARD 3.7 The provider shall have written policies and procedures governing the remuneration and reimbursement of expense-related expenses for planners, faculty, and authors.
STANDARD 3.8 The provider, joint provider, or designated educational partner shall pay directly any teaching or authoring fees or expense reimbursement in accordance with the provider's written policies and procedures.
STANDARD 3.9 No other payment shall be provided to the director, planning committee members, faculty or authors, joint provider, or any other person involved in the supported activity.
STANDARD 3.10 If faculty or authors are listed on the agenda for a presentation or meeting but participate in the rest of the training activity as attendees, their expenses may be reimbursed and honoraria may be paid only for their role as a faculty or author.
STANDARD 3.11 Social events or meals at the above-mentioned events may not compete with or take precedence over educational events.
STANDARD 3.12 A provider may not use commercial support to pay for travel, lodging, honoraria, or personal expenses for participants who are not faculty or authors of CME activities. A provider may use commercial support to pay for travel, lodging, honoraria, or personal expenses for bona fide employees and volunteers of the provider, joint provider, or educational partner.
STANDARD 3.13 The provider must be able to create accurate documents that detail the expenditure and receipt of commercial support.
Standard 4: Appropriate management of associated commercial assistance
STANDARD 4.1 The organization of commercial exhibits or advertising may not influence the planning or interfere with the presentation, nor may it be a condition of commercial support for CME activities.
STANDARD 4.2 Promotional material promoting a product or advertising of any type is prohibited as part of or during CME activities. The juxtaposition of educational and promotional materials with the same products or subjects should be avoided. Live (personalized exhibits, presentations) or sustained (print or electronic advertisements) promotional activities must be kept separate from CME. Printed advertisements and promotional materials will not be posted on CME content pages. Promotional materials and advertisements may appear on the first or last page of printed CME content if these materials are unrelated to the CME content with which they appear and are not paid for by CME sponsoring merchants. Advertisements and promotional materials will not be displayed on the screen at the same time as the CME content.
Also, ACCME-accredited providers may not host their CME activities on a website owned or controlled by commercials. With a clear message that the learner is leaving the educational website, links from the ACCME accredited provider's website to the pharmaceutical and device manufacturers' product websites are permitted before or after the educational content of the CME activity, but must not be displayed in the educational content of the CME activity. Advertising of any type is prohibited in the educational content of online CME activities, including but not limited to banner ads and pop-ups. For electronic CME activities, promotional materials and advertisements may not be displayed on the screen at the same time as the CME content and may not alternate between computer windows or CME content screens. For audio and video recordings, promotional materials and announcements will not be included in the CME. There will be no "commercial breaks". For live, face-to-face CME, advertisements and promotional materials may not be displayed or distributed in the learning space immediately before, during, or after the CME event. Providers may not permit representatives of commercial interests to engage in sales or promotional activities while in the CME space or location.
STANDARD 4.3 Educational materials that are part of the CME activity, such as slides, abstracts, and handouts, may not contain advertising, corporate logo, trade name, or product group message as defined by ACCME as a commercial entity.
STANDARD 4.4 Printed or electronic information distributed about non-CME elements of a CME activity that are not directly related to the education of the trainee, such as descriptions of schedules and other information, may include product promotional materials or product-specific advertising.
STANDARD 4.5 The provider shall not use a merchant as an agent to provide CME activities for learners, such as distributing self-paced CME activities or providing electronic access to CME activities.
Standard 5: Content and format without commercial prohibition.
STANDARD 5.1 The content or format of CME activities or related materials should promote the improvement of the quality of healthcare and not a specific pecuniary interest.
STANDARD 5.2 Presentations should include a balanced list of therapeutic and other treatment options. The use of generic names will promote such impartiality. If educational material or CME content includes trade names, trade names from multiple companies should be used, not just trade names from a single company.
Standard 6: Disclosure of information related to potential commercial prohibition.
STANDARD 6.1 The CME provider shall disclose to the trainees the relevant financial relationship with the commercial entity, including the following information: name of the individual; name of the commercial entity(ies); and the nature of the relationship the provider has with each commercial entity.
STANDARD 6.2 If the CME provider does not have a relevant financial relationship with a commercial entity, the trainees shall be informed of the absence of such a relationship.
STANDARD 6.3 The source of all support from commercial interests shall be disclosed to the trainees. When commercial support is "direct", the nature of the support should be disclosed to the trainees.
STANDARD 6.4 Disclosure should never include the use of the corporate logo, trade name, or product group message of an ACCME-designated commercial entity.
STANDARD 6.5 The provider shall disclose the above information to the trainees prior to the start of the educational activity.



